Home > Blogs > Neurosurgery > Endoscopic Third Ventriculostomy : an Innovation in Neurosurgery
Endoscopic Third Ventriculostomy : an Innovation in Neurosurgery
Hydrocephalus literally means ‘water in brain’, but the term is used to denote an abnormal increase in the water content within the cavities of the brain. This clear fluid, called as ‘cerebropinal fluid or CSF’, is produced within cavities of the brain called ‘ventricles’, circulates within various channels, escapes the ventricles through small holes, bathes the brain surface from outside and gets absorbed in the large veins outside the brain by a special system. CSF is essential for brain functioning and production and absorption are matched.
If, either the circulation or absorption of CSF gets hampered due to some reason, it leads to accumulation of the fluid inside the brain cavities, leading to enlargement of the cavities and pressure on the brain tissue, damaging brain cells, leading to potentially harmful effects – ranging from just headaches to head enlargement, physical incapacity, mental retardation, blindness and death.
Hydrocephalus is known from ancient times and it is supposed to occur in one in 200 live births. Hydrocephalus has many causes dependent on age of patient
- Causes in the pediatric population
- congenital (due to malformations like aqueductal stenosis or due to intrauterine bleeding in the brain
- acquired (complication of trauma, infection or tumour).
- In adults the causes are
- tumours
- late onset aqueductal stenosis
- consequences of trauma
- bleed, infection and normal pressure hydrocephalus.
As far as management is concerned, hydrocephalus is classified according to the mechanism which leads to accumulation of the fluid in the brain cavities –
- Obstructive hydrocephalus – a structural lesion causes hindrance to the flow of CSF, blocking it within the ventricular system, e.g. aqueductal stenosis or a tumour tentorial notch preventing the CSF flow from IIIrd to IVth ventricle.
- Communicating hydrocephalus
- Sometimes, a third, Mixed type is proposed, when the mechanism is poorly or incompletely understood.
Surgeries for relief from this condition are obviously aimed at the drainage of the fluid, have been performed since more than 100 years. They can be grossly divided into external diversion procedures, called shunts (where the fluid is taken out of head with help of a tube and released into abdominal cavity or blood) or internal diversion procedures like ventriculostomy, where ‘stoma’ or opening is created for draining the trapped fluid inside the ventricle to the exterior of brain, to be absorbed by the natural mechanism.
This opening could be done with major open surgery (as was done long ago) or with help of an endoscope, called endoscopic third ventriculostomy, or ETV. This ETV surgery is ideal for most of cases of obstructive hydrocephalus and will be discussed in detail. ETV aims at forming a new pathway for ‘internal’ (intracranial) drainage of CSF, thus bypassing the ‘obstruction’, and hence, is more physiological as against ‘external’ drainage, shunt surgery.
The idea of ventriculostomy itself for the management of hydrocephalus was conceived long ago by one of the great pioneers of neurosurgery, Dr. Walter Dandy in the 1920s. It had fallen out of favour due to high complications mainly because the instrumentation was underdeveloped.

Advances in optical technology, micro-instrumentation, high-resolution imaging and neuroimaging, together with a rising interest in minimally invasive techniques, have resulted in the re-establishment of modern neuroendoscopy and has led to a resurgence of Endoscopic Third Ventriculostomy (ETV).
Today, ETV is the most commonly practised cranial neuroendoscopic procedure.
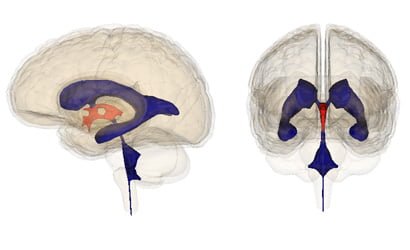
Endoscopic ventriculostomy in action: Diagram on the left shows how aqueductal stenosis causes hydrocephalus, while on the right shows the creation of an alternate channel in the floor of the third ventricle by ETV.
The surgeon first needs to decide which cases to subject for ETV and which for shunt surgery. He should have sound knowledge of the pooled data (evidence base) and be able to apply it to the given case by studying various details (clinical and radiological) of the specific case, using his personal experience and judgment in that given case.
Factors affecting success:
- Mechanism – obstructive or not
- AGE – Concept of Cranial maturation of CSF absorption: – success rate of ETV after 2 years of age is excellent. This is supposedly due to immaturity of the mechanisms responsible for absorption of the fluid at very young age.
- In the pediatric population obstructive hydrocephalus due to aqueductal stenosis and tumours have documented good success rate.
- ETV is more successfully employed in various adult cases of hydrocephalus like secondary obstructive hydrocephalus (due to brain tumour compressing on CSF channels e.g. Pineal tumors, tectal gliomas, posterior fossa tumors, cerebellar infarct) and where removal of the tumour is not feasible. Success rates are up to 90%.
- In adults, the in the late-onset idiopathic aqueductal stenosis (LIAS) success rate is > 80%.
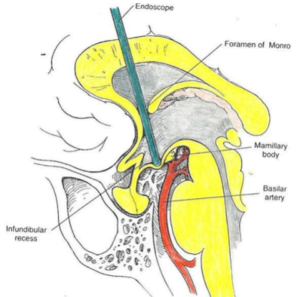
- Anatomical details – practical issues influencing operative steps which need to be studied on imaging, like size of foramen of Monroe, floor of IIIrd ventricle, position of basilar artery etc.
ETV is sometimes also undertaken as conversion of a shunt in a patient who was treated for hydrocephalus as a child:- either the child was less than a year at the time of surgery or simply because ETV was unavailable and now the patient has presented with shunt dysfunction.
Preparation before surgery :
Apart from history and examination, careful study of the imaging is vital in pre-operative evaluation. MRI is the imaging of choice. High resolution MRI also shows small obstructive lesions, presence of blood products or other debris. Sagittal kinematic CINE, phase-contrast MRI can identify absence of flow through the aqueduct.
Why ETV? Is there evidence of supremacy for ETV?
ETV is promoted as a ‘more physiological surgery’ which offers a ‘one time solution’ as compared with the shunt surgery option. The very idea of ETV is of course appealing as it makes patient ‘implant free’ and the surgery is itself an elegant technical challenge (viz. not a resident’s job or not that everyone does). The current consensus states that the incidence of acute complications may be a bit higher with ETV, but a successful ETV eliminates the need for long-term shunting, its attendant morbidity, suffering and the cost that comes with shunt failures.
At the same time, it is folly to think that ETV is a ‘cure’ for each and every case of hydrocephalus. Each surgeon would like to give his patient a permanent solution with minimum risk and complications, and hence, careful patient selection is the key to maximizing the chance of success and minimizing the complication rate.
Technique and instrumentation
One always needs to remember: Minimally invasive ≠ minor surgery! It should only be undertaken in fully staffed and equipped neurosurgical operating rooms and by surgeons who are prepared to tackle its complications and also proceed to an open operation if necessary. Postoperative neuro-intensive care unit (ICU) is a must.
The principle of surgery is to create an internal fistula (passage) between the ventricular system and the area around base of the brain, called basal subarachnoid spaces so as to drain out the fluid trapped inside the ventricles into the subarachnoid system.
The surgeon should be able to appreciate the variations, abnormalities and distortions due to hydrocephalus/lesions and be able to guide the endoscope properly.
Endoscope gives a very high resolution but mono-ocular two dimensional (2-D) view, which is further ’tilted’ (if 30` camera scope is used). So surgeon needs to very well get used to hand-eye coordination.
Surgical steps are simplified for the reader:
As against in open surgery, in endoscopy, only a tiny hole is made into the skull, through which the endoscope is inserted into the ventricles of the brain, navigated from the lateral ventricle into the smaller third ventricle, advanced to the appropriate location at the floor of the third ventricle, where the fistula or stoma is made with help of special instruments.
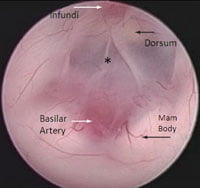


Comparison of a binocular, 3D cadaveric specimen (left) with monocular, 2D endoscopic intraoperative view of the floor of third ventricle. The star ‘*’ indicates ideal site for fenestration.
Perforation is then made in the thinned floor of the third ventricle, allowing egress of cerebrospinal fluid (CSF) out of the blocked ventricular system and into the CSF space outside, but at the base of the brain (a normal CSF space).

A fistula or stoma (opening) is thus created and dilated to sufficient size, CSF flow is confirmed by observing to and fro flapping movements of the lips of the stoma.
Once the patency of the stoma is confirmed, scope is withdrawn and incision is closed. Patient is usually observed in ICU overnight.
Over last 15 years, we have performed close to 100 ETV surgeries and our results are comparable to any top neurosurgical centers in the world. With experience, better case selection and small but important modifications in techniques, our results are even better.
Innovations in neurosurgery should ultimately lead to better quality of life in the patient and especially in case of children “level of reassurance and peace of mind” for their parents.
Have queries or concern ?
About Author
Dr. Charudutt Apte
Neuro Surgeon
Contact: +91 88888 22222
Email – [email protected]
Patient Feedback
Great doctors, Good facilities, caring and helping staff. I recommend this hospital for day care services.
![]()
![]()
Sangram Shinde
All doctors r very good. There treatments is best. Other staff also good. The service of nurses is great...Hospital is always clean.
![]()
![]()
Vaishali Aitawade
All services provide by hospital are nice and on time. Doctors are polite and co-operative with patient.
![]()
![]()
Ankita Jagtap
All services provided by hospital is good. Hygiene maintained well.Even at night good care provided.
![]()
![]()





